Progesterone for Breast Development?
(Author Note: By Popular Demand I Have Updated and Reposted Here My Blog Post on Whether or Not to Take Progesterone.)
Should Male-to-Female Transsexuals Take Progesterone as part of Hormone Therapy (HT) for Better Breast Development?
According to standard WPATH (World Professional Association for Transgender Health) guidelines and upon recommendation from a mental health professional, hormone therapy (HT) is typically an early step for MTF TS to change their bodies including the development of breast tissue. Although some use the term hormone replacement therapy (HRT), the term it is a misnomer because lost hormones are not being replaced as in post-hysterectomy patients. WPATH simply uses the term hormone therapy (HT). HT nearly always involves taking estrogen in some form (e.g. estradiol), may involve testosterone blocking drugs (e.g. spironolactone) and sometimes progesterone (e.g. medroxylprogesterone). The MTF TS should only undertake HT with the oversight of an endocrinologist who has experience in this area and they are rare.
Let me say that I am not an MD and do not purport to give medical advice. Any MTF (male-to-female) TS (transsexual) taking hormones or hormonal blocking agents should be carefully monitored by a qualified endocrinologist. That said, what does the scientific evidence say about taking progesterone as part of MTF TS HT (hormone therapy) with regard to breast development? Clinicians are divided on the subject but there are those MTF TS and doctors who swear it makes a big difference and public information sources support the MTF TS contentions. Transitioning without progesterone and getting breast implants carry their own risks. As with most medical decisions, one has to weigh all the risks with their physician.
Background on Normal Natal Female Breast development.
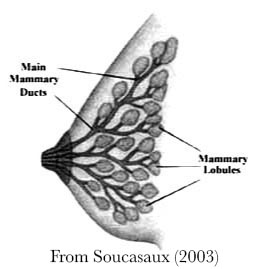
Soucasaux (2003) provides a useful but brief overview of natal female breast development but there are many more online articles. Natal female breast development starts in female puberty that precedes the start of menstruation (menarche). Natal means that the female designation was determined at birth. Breast development proceeds in 5 anatomical stages know as the “Tanner Stages” of breast development (Tanner 1981, 2010) based on nipple and breast structural change.
The two primary tissues in the breast that undergo development are the lobular (milk-producing lobes) and ductwork (milk delivery) tissues. Lobes are made up of clusters of acini (from the Latin for berry because of they form clusters like blackberries on a vine) that are the milk-producing structures. The acini are also called alveoli. During Tanner Stages 1-4 breast development and growth is mediated by estrogen and influences primarily the ductwork tissue. Tanner stage 5 extends into early adulthood and may not be completed until pregnancy.
 When menstruation starts (menarche) progesterone begins to surge on a monthly basis and influences development of lobular structures (Brisken 2002). Progesterone is released in the second half of the menstrual cycle both by from body organs and the corpus luteum, the remnant of the follicle that contained the egg released from the ovary. The surge in progesterone prepares the uterine lining for implantation of the embryo and pregnancy. During pregnancy a bigger and longer surge of progesterone completes breast development and greatly increases breast size in preparation for infant nursing.
When menstruation starts (menarche) progesterone begins to surge on a monthly basis and influences development of lobular structures (Brisken 2002). Progesterone is released in the second half of the menstrual cycle both by from body organs and the corpus luteum, the remnant of the follicle that contained the egg released from the ovary. The surge in progesterone prepares the uterine lining for implantation of the embryo and pregnancy. During pregnancy a bigger and longer surge of progesterone completes breast development and greatly increases breast size in preparation for infant nursing.
Taking progesterone, not only influences breast and body tissues but it also helps reduce testosterone release, just as estradiol does. This is due to a feedback mechanism in the brain that regulates testosterone levels. When testosterone is too low, the brain signals for increased release but when testosterone levels are too high, the brain discourages release.
The PRO-Progesterone Information Sources.
The idea that progesterone is needed for proper breast development seems to come from three sources:
- Numerous public websites, books and articles about normal natal female breast development, indicating a role for progesterone in breast development in girls after menarche during the latter half of the menstrual period; and in women during early adulthood and during pregnancy. Online medical discussions which include debates over the dosage and timing of progesterone administration. Some insist that progesterone should be administered in a manner similar to its release during the natal female menstrual cycle.
- An article (Kanhai et al. 2003) indicating that Ciproterone, a drug with both testosterone-blocking and progesterone-like effects develops lobular breast tissue in MTF TS and thus provides more complete breast development than estradiol alone. (Ciproterone is not generally used for HT in the United States.)
- The rumor that breast development through HT requires progesterone to avoid undesirable “tuberal” breast malformation, although most authoritative sources say that tuberal breast malformation is congenital and is determined by DNA at birth.
I will call out some of these sources during analysis of the most prominent anti-progesterone source which is described in the next section.
The Most Prominent Anti-Progesterone Information Source
There is a prominent clinical article from 2009 that touches on all of the HT breast development issues and which takes a definite stance against using progesterone but is devoid of scientific references. It provides 20 reasons why progesterone should not be used in MTF TS HT. The document was prepared by Dr. Richard Curtis of the London Gender Clinic and published by GIRES (Curtis, 2009) and is still widely distributed through various websites. Curtis runs the London Gender Clinic and is a general practitioner, not an endocrinologist, although his clinic does prescribe for MTF TS HT.
Essentially, Curtis argues that MTF TS individuals should be satisfied with breast size that can be achieved without progesterone (estradiol and testosterone blocker only). This is the maturation and size equivalent to breasts which would be expected in a natal 13.5-year old female prior to menarche. He contends that the risk of taking progesterone is too high compared with the small contribution that progesterone makes to breast development and size. He states that if MTF TS are not happy with the size that can be achieved without progesterone, they should gain weight to increase overall body fat, and consequently breast fat, and/or get breast implants.
The Curtis article contends that progesterone is not only unnecessary for appropriate breast development and growth but should be avoided due the potential risks and gives the following reasons why progesterone should not be used in MTF TS HT:
- The first surge of progesterone in puberty does not occur until after Tanner Stage 5 of breast development is reached at approximately 13.5 years old, so progesterone does not contribute to breast development or size since Tanner Stage 5 is the final development stage.
- Normal breast development up through Tanner Stage 5 and MTF TS HT breast development result in approximately the same bra cup size (A/B)
- Progesterone has unwanted side effects
- The typical dose of progesterone used to manage ovulation or cause abortion is very high compared with what might be expected to be an effective dose if progesterone improved breast size.
- Progesterone antagonizes the effects of estrogen on breast development and size.
- Progesterone converts to testosterone which antagonizes the effects of estrogen on breast development and size.
- Genes influencing the number of estrogen receptors determine resulting HT breast size.
- Breast size growth primarily occurs because estrogen stimulates the growth of ductal tissue and fat, not because progesterone stimulates lobular tissue. Lobular tissue is small in comparison with ductal tissue.
- MTF TS will never breastfeed, so there is no need for breast size development due to progesterone.
- Excessive calorie restriction will interfere with breast size growth.
- Unjustified reasons for taking progesterone include: wanting to experience the same effects that natal females do during menstruation, thinking it will make breasts bigger, wanting to be like your friends (on the Internet), wanting to experience the same effects that natural females do.
- Since menstruation ends at approximately 50, no MTF should take progesterone, since the average age of MTF TS is 42 that is too close to 50 to make it worthwhile.
- Natal females do not like the effects of progesterone.
- Progesterone causes weight gain in MTF TS.
- Well-informed gender clinics do not prescribe progesterone for MTF TS.
- If MTF TS want bigger breasts they should gain weight (“eat more pies”).
- If breast development beyond what would be pre-menstrual growth is desired, the MTF TS can always get breast augmentation surgery which they currently do approximately 50% of the time anyway.
- Breast and nipple tenderness does not indicate breast size growth.
- Too high an initial dose of estrogen is believed to cause conical (I think he means tuberal as in the third Pro-Progesterone information source?) development (Tuberal development means that the breasts develop too narrowly, resulting in a tuber-like shape).
- Although a study showed that a testosterone blocker with progesterone-like effects is needed to have complete breast tissue development, the amount of lobular tissue is so small that it does not have an impact on overall breast size.
Analysis of the Curtis 20 Reasons Why Not Progesterone
So let us consider the 20 Curtis reasons and try to see what science is available to address whether progesterone should be given to MTF as part of HT.
Reason #1. While it is true that estrogen-only breast development occurs until menstruation in natal females, it is not true that progesterone first surges until after Tanner Stage 5 is reached. Levels of estrogen do increase during the start of puberty and breast development (Ankarberg-Lindgren and Norjavaara (2008) while progesterone levels do not (Sippell, W., 1980). However, some sources describe Tanner Stage 5 as being completed around age 15-16, while others say Tanner 5 is not reached until early adulthood or pregnancy (Brisken 2002; Soucasaux, 2003). It is clear that progesterone does contribute to breast development after 13.5 years during the menstrual cycle and that it greatly increases breast development and size during pregnancy. Since progesterone causes an increase in breast size during the latter portion of the menstrual cycle, the average breast size of menstruating females must be somewhat greater than what it was prior to menarche. So this Curtis assertion ignores the role of progesterone in breast development and size and is contradicted by his reason #9.
Reason #2. There is no indication where Curtis got his numbers for cup sizes of TS and natal females. Although bra fitting “science” around the world varies greatly, it is clear that both British (where Curtis practices) and US average cup sizes are much bigger than a B cup, closer to a C or D cup. (Mackay, 2003; http://www.targetmap.com/viewer.aspx?reportId=5285). Thus it would be undesirable to limit an MTF TS to an A/B cup because she would not be perceived as having “average” breasts, particularly those MTF TS who start out with big body frames.
Reason #3. Yes, progesterone has some unwanted potential side effects but the risk of taking estrogens does too. Combination medications of estrogen and progesterone may cause thrombosis or embolism but so do estrogen-only medications; the risk from adding progesterone is unquantified. The jury is still out on whether progesterone protects against or contributes to unwanted side effects of estrogen such breast cancer in post-menopause HT for natal females, although this is a hot research issue because of the large number of postmenopausal females who take HT. Since there is concern about both estrogen and progesterone for thrombosis, MTF TS patients should be warned about embolism and thrombosis symptoms and should be carefully monitored. Some are concerned that taking progesterone reduces bone density but I cannot find any studies on that. But because there is little published data available, MTF TS on HT should be carefully monitored anyway. Bone density scans can now be conducted in a doctor’s office.
Reason #4 There is no scientific data available, that I could find, as to the optimum dosage for breast growth in MTF TS. It is true that current pill dosages were set for menstruation management. Dose titration and monitoring is by an endocrinologist is clearly needed to monitor for side effects.
Reason #5 The indications from scientific data is that progesterone facilitates breast development which contradicts this assertion. Models of breast development show estrogen and progesterone working together (Swerdloff and Ng, (2011). They both encourage release of growth hormone for breast growth and stimulate growth through breast receptors.
Reason #6 It is true that progesterone can be converted to testosterone in both the adrenals and the testes (Steinberger and Fichera, 1968) and it is true that testosterone interferes with the action of estrogen in breast development (Zhou 2000; Hofling 2007) however testosterone blockers usually administered during HT (e.g. spironolactone) should block testosterone effects. Again monitoring testosterone levels by an endocrinologist should prevent testosterone interference from occurring during MTF TS HT.
Reason #7 While it is probably true that genes help determine breast growth in MTF TS HT, there is no data on the subject that I could find. Nor is there any data that supports the idea that the number of hormonal receptors is involved in determining the degree of breast development or size. There is an old tale that MTF TS will have breasts one cup size less than their mother, but there is no evidence available on that point.
Reason #8 Both estrogen and progesterone contribute to breast development with estrogen having primary effects on ductal tissue and progesterone on lobular tissue. Lobular tissue can contribute substantially to breast size (see diagrams in Soucasaux, 2003, above and other breast anatomy sites) especially during natal female pregnancy.
Reason #9 This assertion contradicts earlier assertions by Curtis that progesterone does not contribute to breast development and growth. It is clear that breast development and growth occur during menstruation and pregnancy and that the average breast size of a natal female must be larger than pre-menarche levels.
Reason #10 It is probably true that excessive calorie restriction will prevent breast development and reduce growth size but no one would knowingly advocate such a calorie restriction regimen because of other severe side effects.
Reason #11. There is no scientific data, that I could find, indicating that three of the “unjustified reasons for taking progesterone” given by Curtis are actually articulated by MTF TS. The only one that is probably true is that some MTF TS want to take progesterone to get bigger breasts.
Reason #12 This assertion assumes that MTF take progesterone to mimic menstruation feelings that was already rejected in reviewing assertion #11. Since many postmenopausal natal females take progesterone for well being and to maintain breast health, this is an unjustifiable reason.
Reason #13 No data is available as to whether natal females detest the effects of progesterone. Curtis mentions lots of adverse side effects but there may be other effects that are positive.
Reason #14 There is no scientific data available as to whether progesterone causes weight gain during MTF HT and it is not clear whether this is an negative effect. It is true that estrogen causes changes in weight distribution.
Reason #15 This assertion is an “argument from authority” that knowledgeable European gender clinics do not prescribe progesterone for MTF TS HT treatment. It would have more value if we knew the knowledge that the clinics have which convinces them not to prescribe progesterone HT. In a US survey of 40 gender clinics with 20 responding, 25% were prescribing progesterone (Meyer et al. 1981) but there is no indication as to why or why not a given clinic did or did not prescribe progesterone.
Reason #16 Because of the adverse effects of weight gain on health, unless a person is very underweight, they should not be told that for bigger breasts “eat more pies”.
Reason #17 This assertion assumes that Curtis has concluded that breast augmentation is less risky and has no adverse effects compared with taking progesterone during MTF TS HT treatment. This is an unwarranted assumption since breast augmentation surgery has many risks including implant rejection, autoimmune effects, chronic pain and loss of nipple sensitivity (Pitanguy, 2007; vanElk, et al. 2009 Kaasa, T. et al. 2010; Araco, A. 2011). Patients should know all the risks and rewards of any course of treatment including not using progesterone. Not using progesterone may result in the need for breast augmentation that is already at an undesirable % 50 rejection rate and may reoccur during a lifetime. These decisions should be based on effects-based scientific evidence not just clinical opinion.
Reason #18 There is no scientific data that I could find to dissociate breast development from breast tenderness. Breast tenderness does occur in the second half of the menstrual cycle in natal females due to progesterone with accompanying development of milk-production lobular tissue but it also occurs during the first half of the menstrual cycle because of estrogen.
Reason #19 There is no scientific data that I could find to support the assertion that too high an initial dose of estrogen causes tuberal breast development. The origin of tuberal development of breasts is unknown but is believed to be congenital and there are no reports that I could find that it is more frequent in MTF TS than in natal females. Monitoring by a competent endocrinologist should pick up this problem early in HT and it can ultimately be corrected surgically. Most of the scientific papers on this subject are by plastic surgeons that provide surgical solutions (Panchapakesan and Brown, 2008).
Reason #20. The article mentioned in this Curtis reason #20 is probably Kanhai et al. (2003).This article indicates that a testosterone blocker, ciproterone, which has prostesterone-like effects, in combination with estradiol, was required for lobular breast development in MTF TS HT based on microscopic examination of breast tissue. This supports an earlier study that made the same conclusion (Orentreich and Durr, 1974) without formal microscopic examination. As previously indicated lobular tissue represents a considerable volume of breast tissue particularly during the latter part of the menstrual period and pregnancy.
Bottom Line on the Curtis Article
In an abundance of caution, Dr. Curtis concludes that the risks outweigh the benefits of progesterone for MTF TS HT breast development and size. Dr. Curtis has decided that MTF TS breast growth should be restricted to a growth level similar to a pre-menarche female (approximately 13.5 years old) using only estrogen and testosterone blockers. However, his arguments tend to obscure the fact that progesterone could contribute to enhanced breast development and growth beyond this level.
Conclusion
So should MTF TS take Progesterone as part of HT? The answer, like a lot of medical decisions, is that endocrinologists and patients should discuss the risks and benefits and make a decision and then to carefully monitor the results. To include progesterone in MTF TS HT runs the risks of potential serious side effects. To not include progesterone runs the risk of having unsatisfactory breast development that leads to the breast augmentation surgical risks including loss of sensitivity and pain (Pitanguy, 2007; vanElk, et al. 2009 Kaasa, T. et al. 2010; Araco, A. 2011). The 50% risk of needing to have breast augmentation is clearly too high. There is not currently enough information to make these decisions with formal quantified risk assessments because of the dearth of published scientific evidenced-based research. We can, with some certainty, rule out advice to otherwise non-underweight MTF TS patients to gain weight in order to have bigger breasts because of the well-established risks of being overweight. At the risk of repeating, given the dearth of research results and the resulting unquantified risks, we can conclude with great certainty that MTF TS HT should not be undertaken without careful monitoring by an endocrinologist experienced in this area. According to WPATH, this includes monitoring of testosterone, estrogen, progesterone and prolactin in addition to other tests.
Finally, we ought to be researching and considering new, innovative approaches to MTF TS transition such as:
- Should progesterone be given on a menstrual-cycle-like schedule during HT to mimic natal female development? (I am told some do-it-yourselfers and doctors advocate such an approach.)
- Should progesterone be given after several years of non-progesterone HT when estrogen development stops, just as natal female breast development occurs with menstrual and pregnancy progesterone? This would require objective measurement of breast size and growth that is not consistently done at present. Cup size is just too inaccurate. Breast “sizers” (Pitanguy, 2007) or laser metrology may do the trick.
- Should HT be the initial part of transition? Why not just start with breast augmentation without hormones, followed by Genital Plastic Surgery (GPS) and then HT? (Other terms for GPS are misnomers including sexual reassignment surgery, gender confirmation surgery and gender reconstruction surgery because sex organs are only partially changed and gender has nothing to do with altering sex organs.) This would reduce the potential risks from testosterone blockers. This compatible with WPATH guidelines and has already been use with some patients.
References
Ankarberg-Lindgren, C. and Norjavaara, E. A purification step prior to commercial sensitive immunoassay is necessary to achieve clinical usefulness when quantifying
serum 17b-estradiol in prepubertal children. European Journal of Endocrinology (2008) 158 117–124. http://www.ncbi.nlm.nih.gov/pubmed?term=A purification step prior to commercial sensitive immunoassay is necessary to achieve clinical usefulness when quantifying serum 17b-estradiol in prepubertal children
Araco, A., (2011) Sensitivity of the Nipple-Areola Complex and Areolar Pain following Aesthetic Breast Augmentation in a Retrospective Series of 1200 Patients: Periareolar versus Submammary Incision. Plastic and Reconstructive Surgery Volume 128, Number 4.
Brisken, C. (2002) Hormonal Control of Alveolar Development and Its Implications for Breast Carcinogenesis Journal of Mammary Gland Biology and Neoplasia, Vol. 7, No. 1, January 2002 page 45
Curtis, R. (2009) The Lowdown on Progesterone, http://www.gires.org.uk/assets/Medpro-Assets/Progesterone.pdf
Kanhai, R. et al. The American Journal of Surgical Pathology 24(1): 74–80, 2000
Hofling M. Testosterone inhibits estrogen/progestogen-induced breast cell proliferation in postmenopausal women. Menopause. 2007 Mar-Apr; 14 (2): 183-90. http://www.ncbi.nlm.nih.gov/pubmed?term=Testosterone inhibits estrogen%2Fprogestogen-induced breast cell proliferation in postmenopausal women.
Kaasa, T. et al. (2010) Hyperesthesia one year after breast augmentation surgery increases the odds for persisting pain at four years A prospective four-year follow-up study Scandinavian Journal of Pain 1 75–81
Kanhai, R. et al. (2000), Short-Term and Long-Term Histologic Effects of Castration and Estrogen Treatment on Breast Tissue of 14 Male-to-Female Transsexuals in Comparison With Two Chemically Castrated Men, The American Journal of Surgical Pathology 24(1): 74–80.
Mackay. J. (2000) Atlas of Human Sexual Behavior, Penguin.
Meyer, W. et al. (1981) A Survey of Transsexual Hormonal Treatment in Twenty Gender-Treatment Centers, The Journal of Sex Research, Vol 17, No.4. pp 344-349.
Orientreich, N. and Durr, N. (1974) Mammogenesis in Transsexuals. The Journal of Investigative Dermatology. 63. 142-146. http://www.ncbi.nlm.nih.gov/pubmed?term=Mammogenesis in Transsexuals. The Journal of Investigative Dermatology
Panchapakesan, V. and Brown, M. (2008) Management of Tuberous Breast Deformity with Anatomic Cohesive Silicone Gel Breast Implants Aesthetic Plastic Surgery Volume 33, Number 1, 49-53 http://www.ncbi.nlm.nih.gov/pubmed?term=Management of Tuberous Breast Deformity with Anatomic Cohesive Silicone Gel Breast Implants
Sippell, W., et al., 1980,Plasma levels of aldosterone, corticosterone, 11-
deoxycorticosterone, progesterone, 17-hydroxyprogesterone, cortisol, and cortisone during infancy and childhood. Pediatric Research. 1980 Jan; 14(1): 39-46. http://www.ncbi.nlm.nih.gov/pubmed?term=Plasma levels of aldosterone, corticosterone, 11- deoxycorticosterone, progesterone, 17-hydroxyprogesterone, cortisol, and cortisone during infancy and childhood
Pitanguy, I. et al. (2007) Relative Implant Volume and Sensibility Alterations After Breast AugmentationAesth. Plast. Surg. 31:238–243.
Soucasaux, N. (2003) The Breasts: Some Morphological Aspects. http://www.mum.org/thebreas.htm
Steinberger, E. and Fichera, M. (1968) Conversion of progesterone to testosterone by
testicular tissue at different stages of maturation Volume 11, Issue 3, March 1968, Pages 351-368 http://www.ncbi.nlm.nih.gov/pubmed?term=Conversion of progesterone to testosterone by testicular tissue at different stages of maturation
Swerdloff, R. and Ng, J. (2011) Gynecomastia: Etiology, Diagnosis, and Treatment http://www.endotext.org/male/male14/male14.html
Tanner, J. (1981, 2010) A History of the Study of Human Growth, Cambridge Press
vanElk, et al. (2009) Chronic pain in women after breast augmentation: Prevalence, predictive factors and quality of life. European Journal of Pain 13 660–661.
Zhou, J. et al. (2000), Testosterone inhibits estrogen-induced mammary epithelial proliferation and suppresses estrogen receptor expression. The FASEB Journal Vol. 14 September 2000, 1730. http://www.ncbi.nlm.nih.gov/pubmed?term=Testosterone inhibits estrogen-induced mammary epithelial proliferation and suppresses estrogen receptor expression
Dana Bevan looks further into hormones for breast development with Grow Your Own : Breast Development Update published in January 2019.
Category: Transgender Body & Soul



